Measuring Student Knowledge and Curriculum Comprehension With ‘Desire 2 Learn’
In the Pikes Peak Community College Surgical Technology Program, student knowledge and curriculum comprehension are measured in a few ways. The one that has become a point of interest within our department is the way we analyze students' computer-based quizzes taken in class at the end of each chapter.
Meet Your Newly Elected ARC/STSA Board’s Executive Committee Members
The ARC/STSA Board of Directors recently elected three members to its Executive Committee: Janice Grewatz (president), Erin White-Mincarelli (vice president) and Ron Ehlers (secretary/treasurer). Get to know them in this feature.
ASA Annual Meeting Recap
The Association of Surgical Assistants (ASA) recently hosted its fall workshop and annual meeting in Phoenix, Arizona, September 24-25, which was packed with informative speakers, hands-on workshops and networking opportunities for the 65 surgical assisting practitioners and educators in attendance.
A Round of Applause to Initially Accredited Programs
ARC/STSA would like to congratulate the surgical technology programs at Altierus Career College, Ivy Tech Community College, Long Island University, Silicon Valley Surgi-Tech Institute, South College and Suffolk County Community College for receiving initial accreditation. Please join us in acknowledging the dedication and hard work it took for these programs to reach this milestone.
Tell Us How You Celebrate 50 Years
ARC/STSA is celebrating 50 years of excellence in 2022! Is your organization celebrating a 50th milestone? We want to hear about it!
Message From the Executive Director: Updates to Keep on Your Radar
With summer coming to a close, I hope that you all were able to take some well-deserved time off to relax and recharge. This year is rushing by at a frantic pace, and there is much to update you on from the world of accreditation.
Planning Your Year: A Program Director’s Tips for Time Management
Thirteen years ago, I made the decision to transition from working in the operating room to teaching full time with only a year of experience as an adjunct educator. Like most of my colleagues, I came straight out of the clinic with only a fraction of what I needed to succeed.
Creating Interactive Education: A SoftChalk Success Story
2020 was a challenging year for surgical technology instructors, with many having to quickly retool their courses and shift to distance education delivery. Some became Zoom experts and provided synchronous lectures while others used their college’s learning management system (LMS) to deliver course materials.
Get to Know Your New ARC/STSA Board Members
The ARC/STSA Board of Directors recently welcomed two new members, Eboni Saurage, EdD, CST, and Jay Chambers, BS, CST.
‘I Choose to Never Quit’: 2021 Chris Keegan Memorial Educator Scholarship Winner Shares Her Story
The ARC/STSA Chris Keegan Memorial Educator Scholarship is awarded to surgical technology and surgical assisting educators pursuing academic degrees with the goal of furthering their career in the field of surgical technology or surgical assisting education. 2021 scholarship recipient Kendra Thompson, ST-R, CST, shares her story.
A Memorable Experience: 2021 AST Conference Student Attendees Share Their Takeaways
The 2021 Association of Surgical Technology (AST) Conference took place July 21-23 in Las Vegas, NV. Christopher Achim and Edison Smith, student attendees from the Nevada Career Institute, Las Vegas, share their key takeaways from the memorable experience, including their favorite sessions, an overview of the student forum and the importance of attending an event of this magnitude early in their professional careers.
Just Launched! Visit Our New EdAccred Website
ARC/STSA is proud to announce the launch of the EdAccred website (Edaccred.org), with resources designed to support surgical technology and surgical assisting educators.
Creative DIYs for Simulation-Based Training
As educators, we bring a lot of creativity to our training, coming up with hacks, tips and tricks to demonstrate surgical procedural skills. We also know that hands-on, simulation-based training is one of the best ways to engage students and prepare them for entering the field. As program director, I look for simulation tools and training platforms that give me room to be creative.
How to Onboard Your Students for a Clinical Rotation
One of the most important tasks when I begin a cohort is assigning my students to a clinical site. In years past, this process was completed with a few emails. However, many hospitals are now keeping track of their clinical students through an online onboarding service. These websites have given hospitals the ability to access all student information in one place, which has made it much easier for hospital staff to coordinate their clinical rotations.
Drive-Through, Livestream and Zoom Commencements: Surgical Technology and Surgical Assisting Programs’ Creative Twist to Pomp and Circumstance
Graduation for the class of 2021 (and 2020) presented many programs with a challenge: How should graduation ceremonies balance safety and celebration? We asked surgical technology and surgical assisting educators how their institutions approached the situation and were wowed by their dedication and creativity. Take a look in this round up of stories from across the country.
What OR Leadership Wants From Surgical Technologists in Training
A student’s first rotation as a surgical technologist can be daunting. As educators, we want to prepare students as best we can for the operating room. But what does the operating room expect from surgical technology students? To find out more, I asked a nurse manager and an operating room (OR) educator from two different hospital systems what they expect from a surgical technology clinical student.
Highlights From the Second Annual ASA/NSAA Conference
Surgical professionals from across the country gathered for the second annual Joint Conference of the Association of Surgical Assistants (ASA) and National Surgical Assistant Association (NSAA), April 23-24 in Orlando, FL. The two-day event included hands-on learning experiences, inspiring speakers, legislative insights, and an opportunity to network with colleagues and exchange ideas.
Congratulations to ARC/STSA 2021 Scholarship Recipients!
The ARC/STSA is proud to announce the recipients of the 2021 scholarship awards. This year, ARC/STSA awarded 10 student scholarships of $500 each and one $1,000 educator scholarship. Join us in celebrating these accomplished recipients, shared below, and stay tuned for more information about their stories throughout the summer.
Three Cheers for Programs Earning Initial and Continuing Accreditation
ARC/STSA would like to congratulate the surgical technology programs at Wallace Community College, Marion Technical College and Blackhawk Technical College for receiving initial accreditation, and Augusta Technical College for receiving continuing accreditation. Please join us in congratulating these programs for achieving this accomplishment and acknowledging the dedication and hard work it took to reach such important milestones.
A Patient-Driven Simulation: A Look at the Cut Suit
From virtual simulation to synthetic cadavers and more, surgical technology and surgical assisting programs are incorporating the very latest in innovative, hands-on training activities into their curricula. The Cut Suit is a simulation tool that is worn by a live human and replicates the look and feel of traumatic injuries. Designed by surgeons for surgeons, the Cut Suit allows students to practice for high-pressure situations with room to safely make non-life threatening errors.
Why One Nebraska Program Launched a Certificate for Surgical First Assistants
Southeast Community College (SCC) in Lincoln, NE, recently launched a certificate program for students looking to become surgical first assistants (SFAs). Hear from Program Director Cynthia Kreps on what drove this decision and how launching the certificate has benefitted their college and community.
Think Outside the Book: Swatting for Success
How do we get students out of their seats and actively engaged in the classroom? Most instructors ponder this question for course content outside the laboratory setting. At Trine University’s Surgical Technology Program, flyswatters are a key to successfully helping student better engage in their learning experience. This common household item is useful for not only test review sessions, but also for team bonding amongst the students.
In Memory of Karen Ludwig
It is with a profound sense of loss that ARC/STSA says goodbye to Karen Ludwig, BA, a beloved member of the surgical education community, who passed away on February 11, 2021. Ludwig was born on October 24, 1945, near Chicago and received her bachelor’s degree in English from the University of Colorado. She worked at AST for more than 20 years in various capacities, primarily serving during that tenure as director of publications.
Celebrating All Things SA: ASA-NSAA Conference and SA Appreciation Week
The second annual Joint Conference of the Association of Surgical Assistants and National Surgical Assistant Association will take place on April 23-24 in Orlando, Florida. The conference will offer a range of workshops, exhibitions, discussions and more on emerging trends in the world of surgical assisting.
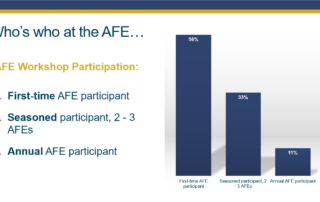
AFE Workshops Continue, Bringing Educators Together
The February and March Virtual AFE Workshops were a roaring success! Co-presented with ARC/STSA’s education initiative, EdAccred, the events drew a range of new and seasoned program directors, clinical coordinators, instructors and administrators. Interested in a future workshop and wondering where you fit in? Take a glance to learn who’s who at the February AFE.

Surgical Technology Sequencing for Student Success
By Melanie Graves, MBA, CST
In surgery, precision isn’t optional — it’s vital. Every member of the operating room team must be efficient, alert and disciplined. Surgical technologists play a key role in this critical environment, and the way they are trained matters. Our program uses a step-by-step, sequential training approach that gives students the knowledge, skills and confidence to succeed — not just in class, but in the operating room as well. When the teaching method is built around aseptic technique, timely clinical placements and well-integrated observation experiences, it doesn’t just build better techs — it protects patients.
First Semester: Building a Strong Foundation
In our surgical technology program, the first semester is carefully structured to focus on foundational skills, without introducing specialty cases. Students begin by learning the core principles of asepsis — the backbone of surgical safety. At this stage, the curriculum follows a strict sequence. Students progress from understanding what a preference card is to learning how to pull a case, mastering the names of instruments, opening a surgical case, perfecting how to scrub, gown and glove, and preparing a basic exploratory laparotomy.
This approach ensures that students understand not only what to do but why it matters. Aseptic practices aren’t just skills to memorize — they are life-saving measures. Teaching them early and thoroughly helps students develop discipline, attention to detail, and the mindset needed for surgical teamwork.
Observation Clinicals: Bridging the Gap
While mastering these foundational steps, students also attend a weekly observation clinical rotation. These observation days are intentionally placed during the first semester — after core concepts are taught but before hands-on clinicals begin. This timing allows students to see the surgical environment in action, reinforcing what they’re learning in the classroom and lab.
During these observations, students watch surgical teams perform live procedures. They learn how sterile technique is maintained under pressure, how team members communicate, and how the flow of a surgery unfolds in real time. Just as important, they see where to stand, learn when to speak and how to respect and preserve the sterile field.
This early exposure shapes their understanding of the OR, ignites curiosity and builds motivation. When they return to the lab, they bring better questions and sharper focus, connecting classroom knowledge to real-world practice.
Clinical Readiness Exam: The Gatekeeper to Clinical Practice
Before students can begin their hands-on clinical rotations, they must pass a comprehensive final hands-on skills assessment called the Clinical Readiness Exam. This exam is designed to ensure that students have mastered essential competencies: setting up sterile fields, identifying instruments, maintaining asepsis, and demonstrating confidence in the basic sequence of surgical case preparation.
This high standard protects both students and patients. Clinical sites expect students to be capable, prepared and safe. Requiring mastery before placement ensures that students enter the OR as contributors, not as liabilities.
Specialty Cases Come After the Basics
Only after passing the Clinical Readiness Exam do students transition into their clinical rotations, where the focus shifts to specialty surgeries. This timing is intentional. By this stage, students are no longer in the learning phase of how to handle instruments or keep a sterile field — they’ve already mastered those skills. Now, they can focus on learning the nuances of various specialties such as orthopedics, neurology, gynecology and more.
This sequence allows students to absorb complex information in context. They’re not distracted by basic technique or overwhelmed by unfamiliar environments. Instead, they’re ready to adapt, assist and grow into the role of surgical technologist with confidence and clarity.
Structured Training, Stronger Technologists
When surgical technology is taught in a well-ordered, sequential format — grounded in aseptic principles, supported by observation clinicals and timed appropriately for hands-on practice — the results speak for themselves. Students gain more than technical ability. They learn to think critically, act decisively and uphold the safety of the surgical field with integrity.
They understand the “why” behind every step, understand the connection to the “how”, and they’re equipped to support the surgical team from day one. From their first semester to their final rotation, they develop into professionals who are prepared, capable and committed to patient care.
Conclusion
Surgical technology is a discipline where preparation, precision and patient protection intersect. Teaching it in sequential order — with aseptic technique as the foundation, early observation as reinforcement, and clinical placements timed after demonstrated readiness — transforms students into professionals. In our program, students learn the basics first, master their skills in the lab, and only then enter the clinical field to explore specialty surgeries. This structure produces not only skilled technologists but also thoughtful, reliable team members who understand their vital role in safeguarding patient lives.
Melanie Graves, MBA, CST, is the Program Director and Department Chair of Surgical Technology at Austin Community College in Austin, TX. She graduated from the same program in December 2015 and scrubbed in Austin and Cedar Park until 2022. In January of 2020, she began teaching for ACC’s Surgical Technology program alongside those who taught her, and she moved into her role as the Program Director in August of 2023.