By Rob Blackston, M.Ed., CST, CSFA, FAST
The surgical technologist staffing shortage is a serious issue that can have a significant impact on patient care and safety. It is essential to address this shortage by increasing the availability of, and access to, education programs that attract and retain more individuals in this field.
A few months ago, a local community not-for profit healthcare system enlisted my support to address staffing challenges. Initially, the hospital administrators had envisioned a “grow your own,” on-the-job trained (OJT) “surgical technician” program to potentially “solve their staffing issues”. With the workforce shortage of surgical technologists, among other healthcare professionals, hospitals and surgery departments across the country are faced with the cascading effects of low staffing, such as closed rooms, a reduction in surgeries, a decrease in monetary inflow, and practitioner burnout. These pressures can become perpetuating issues that can lead to a lower standard of care, due to cutbacks of essential resources.
As a steadfast advocate of standardized, quality education for our profession, I sought to explore alternatives incorporating nationally recognized standards of surgical technology education to present to hospital administrators. From this research and exploration, the win-win concept of a Surgical Technology Residency Program was born.
Surgical Technology Residency Program
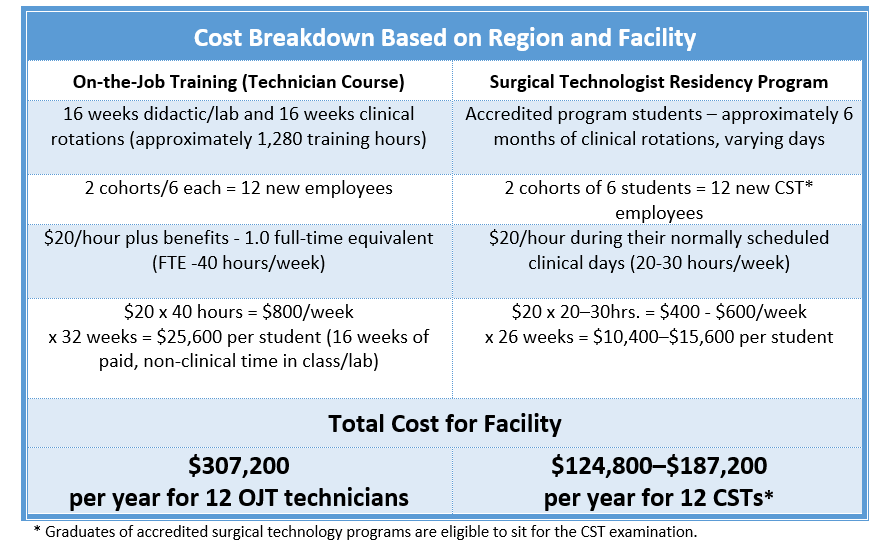
The residency program is a collaboration between healthcare organizations and education institutions to develop a comprehensive approach that can meet the demands of the industry while providing safe and effective patient care. It provides the hospital with well-educated (CST-eligible) surgical technologists, financial support for the participating students, AND saves the hospital more than $100,000 over training those same students on the job.
The hospital’s original plan was to train two cohorts of six students on-the-job as surgical technicians, per year. It would pay the OJT students a fulltime “student wage” to attend the hospital program and then hire them into a fulltime ST role (Washington does not require certification). As an alternative solution, I designed the ST Residency Program and proposed that we form two cohorts comprised of students from the region’s accredited surgical technology programs.
To secure approval for the program and enlist the support of hospital administrators who may not fully understand the complexity and critical nature of our role in the operating room, it was important to articulate the program’s monetary benefit as well. Providing rough calculations to compare the costs of two options seemed to speak volumes. Let’s take a look at the numbers.
Surgical Technologist Residency Program Description
The hospital will accept six ST Residents twice a year. These positions are advertised by the hospital and open to ALL students who:
- Are currently enrolled in a CAAHEP- or ABHES-accredited Surgical Technology program;
- Have successfully completed and documented basic lab skills checkoffs and qualify for clinical rotations, based upon individual program requirements and Program Director approval; and
- Are documented in good standing with their program (no disciplinary action in progress or failing grades).
ST Residency Program applicants will be interviewed by a panel of hospital staff and selected utilizing a residency program interview rubric. Resident students will adhere to their individual program requirements and oversight by program faculty will still be required. For example, if a program requires more than the minimum curricular case count, then that is what the student will work to complete.
Resident students will progress through clinical cases and specialties in a logical progression that builds on their progressive mastery of skills, as the surgery schedule allows, and will have frequent evaluations by both staff preceptors and program faculty (as noted in their individual programs).
To provide support and consistency, the hospital will institute a ST preceptor development program. This program will serve to identify quality preceptors, develop their skills, and give the preceptors the tools to ensure an optimal student/preceptor experience.
Summary
Addressing the surgical technologist staffing shortage requires collaboration between healthcare organizations and education institutions to develop a comprehensive approach that can meet the demands of the industry while providing safe and effective patient care. The Surgical Technologist Residency Program capitalizes on paid student internships to help address the workforce shortage, and benefit the student, healthcare facility, community, and surgical patient.
Call to Action: Continue to educate the public and inspire your local CSTs to get out there and recruit for your programs. Encourage the leaders of our profession to be forward facing to the public and invest time into advertising our profession. Get the word out! If the average person doesn’t know about the profession, how can we grow? How can we expect them to understand the importance of our role, so they don’t think that they can just do a quick OJT course? Aeger primo!
“Better is possible. It does not take genius. It takes diligence. It takes moral clarity. It takes ingenuity. And above all, it takes a willingness to try.” ― Atul Gawande, Better: A Surgeon’s Notes on Performance
Editor’s note: The CAAHEP Standards and the ARC/STSA do allow for paid student clinical activities provided that the experience is educational in nature, students are not substituted for staff, and the health and safety of the students, patients, faculty and other participants associated with the educational activities of the students are adequately safeguarded.
 Rob Blackston, M.Ed., CST, CSFA, FAST, is the Supervisor of Clinical Education – Surgical Technology at Providence – Sacred Heart Medical Center in Spokane, WA. With more than 18 years as a practicing CST and CSFA, Blackston has scrubbed and assisted in all specialties but is not shy about expressing his love for the neurosurgical and orthopedic specialties. Blackston has been an educator for more than 12 years, having served as the program director for surgical technology programs in Idaho and Montana and most recently, starting a new surgical technology program at North Idaho College, in Coeur d’Alene, ID.
Rob Blackston, M.Ed., CST, CSFA, FAST, is the Supervisor of Clinical Education – Surgical Technology at Providence – Sacred Heart Medical Center in Spokane, WA. With more than 18 years as a practicing CST and CSFA, Blackston has scrubbed and assisted in all specialties but is not shy about expressing his love for the neurosurgical and orthopedic specialties. Blackston has been an educator for more than 12 years, having served as the program director for surgical technology programs in Idaho and Montana and most recently, starting a new surgical technology program at North Idaho College, in Coeur d’Alene, ID.
Blackston served as ARC/STSA Accreditation Manager from April 2022-January 2023 and has served for more than 10 years as an ARC/STSA site visitor, and has also served on the Montana AST State Assembly’s Board of Directors and the Idaho AST State Assembly as President. He has served as a panel member for the Core Curriculum for Surgical Technology, Seventh Edition, a member of the AST Education and Professional Standards Committee, and has been a contributor and reviewer for numerous surgical technology textbooks. In 2021, he was awarded the Fellow of the Association of Surgical Technology (FAST) designation.
Blackston earned his Master of Educational Technology, with a certificate in Online Teaching, from Boise State University, in 2018. He was awarded the Carolyn Thorson departmental award for excellence in educational technology and graduated with honors.